Raymond Berry was one of the first patients to benefit from a new service being used at The James Cook University Hospital to detect and monitor oesophageal conditions such as Barrett’s cancer.
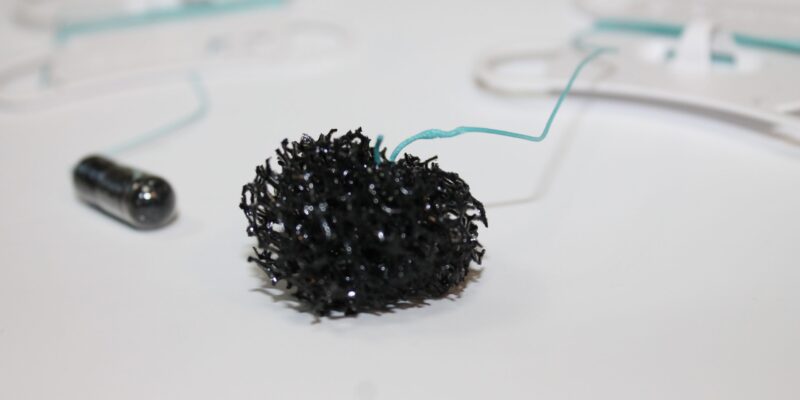
The new Cytosponge is a small capsule which is attached to a string.
Patients like Raymond are asked to swallow it while the nurse keeps a hold of the string. Its outer lining, made of vegetarian glutelin, then dissolves to reveal a tiny sponge around the size of a 10p piece.
The sponge is withdrawn from the stomach via the mouth by a quick pull of the string, taking between 500,000 and 1 million cells on its way before it is sent to the lab for examination.
Raymond, a former miner from near Loftus, has regular endoscopies after pre-cancerous cells were previously found in his oesophagus.

“Usually, I have the endoscopic camera but obviously this is a new treatment and I said I’d volunteered to have it done and it was easy, better than the camera,” said the 66-year-old.
“I’ve had the endoscopic camera six times but compared this is better, it isn’t stressful.
“When they said they’re going to put a tablet down in your mind you have a good idea what it is, but the tablet I thought would be bigger. It was only a small tablet but when it came out it’d obviously swelled up.
“I’d tell others not to worry if they’re having this because it’s what seven minutes, seven and a half minutes and they pull it out gradually, you get a bit of wind but nothing else. I just hope it helps everybody else.”
Arvind Ramadas clinical lead for endoscopy said: “The early detection of cell changes (dysplasia) in Barrett’s oesophagus could make treatment much easier and enable doctors to intervene before cancer develops.
“This procedure will be rolled out in a phased manner through the South Tees minimally invasive gastrointestinal service.”

Peter Davis, consultant upper GI cancer surgeon and chair for the regional cancer MDT, added: “I’m delighted that South Tees has become an early adopter of this new diagnostic approach and technology.
“This will allow the diagnosis of oesophageal cancer patients at an earlier stage with improved outcomes.”
Leila Lyons, nurse endoscopist added: “This is another exciting development within our department.
“It enables us to perform essential assessments of patients who we know are at risk of oesophageal cancer in a less invasive and less stressful way.
“The patients we have seen so far have found it a much easier test than the scope, it’s quick, comfortable and they can return to their normal activities right away.”