Endoscopy

This leaflet describes the purpose of your procedure and what is involved for you. Please read this carefully before coming for the procedure so that you can be reassured about what will happen when you attend the Endoscopy unit.
Outpatient test – This leaflet should provide you with the all the basic information about the test.
- Some patients are referred directly for a Colonoscopy by their GP or a hospital clinician. In addition to this leaflet, you will be given the opportunity to ask any questions about the procedure.
- Other patients will have been given the opportunity to ask any questions about the procedure when attending either an outpatient clinic appointment before the test or at the hospital pre-assessment visit.
Despite this, occasionally questions about the procedure remain. If you have any major concerns before then you should contact us using the contact details at the end of this leaflet.
In-patient test – The medical and nursing staff responsible for your care will be able to answer your questions regarding the procedure.
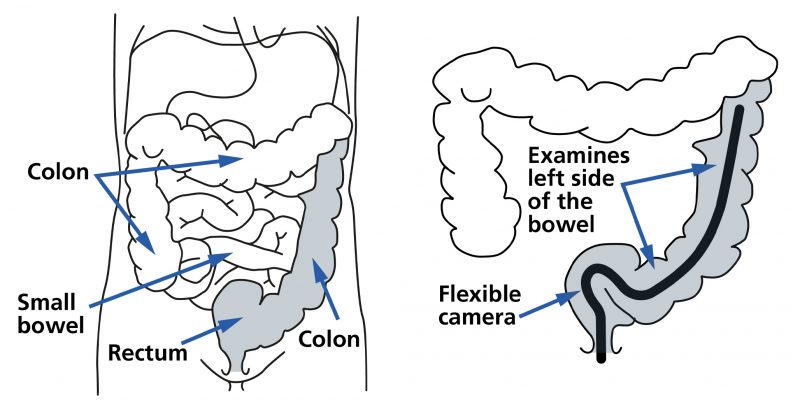
What is a flexible sigmoidoscopy?
A flexible sigmoidoscopy is a procedure which allows the endoscopist (person performing the colonoscopy) to look at the lining of the left side of the colon (large bowel). This is done by passing a long flexible tube (the thickness of your index finger) through the anus and into the bowel. Gas is blown into the colon to achieve a clear view.
The procedure usually takes approximately 15-20 minutes but your total expected stay could be up to four hours. You should be aware that occasionally investigations may be delayed if emergency cases occur.
How may a flexible sigmoidoscope help?
This examination allows the endoscopist to obtain a very clear and thorough inspection of the left side of your colon and take pictures of the bowel for your flexible sigmoidoscopy report. A flexible sigmoidoscopy is often undertaken when someone has one or more of the following:
- Some types of abdominal pain.
- Noticeable rectal bleeding from the back passage.
- Rectal symptoms such as localised pain and itching.
- Assessment or removal of lesions such as polyps (benign growths) known to be in the left side of the large bowel.
- Known large bowel conditions, such as colitis, affecting the left side of the large bowel.
- A previous history of colorectal cancer where a significant portion of the large bowel has been removed.
Diseases of the colon can either be ruled out or diagnosed accurately. In many cases it may be appropriate to take biopsies (small samples of tissue). These are taken using tiny forceps and are sent to the laboratory. Taking biopsies is painless and very safe. It may also be necessary for the endoscopist to remove polyps (small benign growths) from the lining of the colon.
Is there an alternative?
Some assessment of the left side of your colon can be achieved using an ultrasound scan (similar to the type of scan that pregnant ladies have) or a CT scan which produces 3-dimensional images of the abdomen and pelvis with an associated dose of radiation.
Unfortunately, standard ultrasound and CT scans do not identify problems in the lining of the upper Gastro-intestinal tract well and are not really a useful test to identify or rule out most problems in this area. They can sometimes be helpful when the exclusion of a very advanced serious problem is all that is required.
Not having a flexible sigmoidoscopy or an alternative test would limit your doctor’s ability to confirm the cause of your symptoms or condition. You should discuss this very carefully with your doctor. If you decide against having your procedure, then please let the administrative team know so that the valuable appointment can be given to someone else.
You could decide not to have investigations performed but this may mean that your doctor will not be able to diagnose the cause of your problem.
What preparation is required?
When you get your appointment
Please review the medications you take well in advance of your procedure. If you take any of the following medications then please contact us using the contact details at the end of this leaflet.
- Anticoagulant medications to thin the blood (Warfarin, Dabigatran, Rivaroxaban, Apixaban or Edoxaban) or anti-platelet drugs (Clopidogrel, Prasugrel or Ticagrelor). Some of these need to be stopped before endoscopic procedures and some require additional treatment if they are to be omitted.
- If you are a diabetic on treatment with tablets or insulin. Special arrangements are necessary if you need insulin.
You should expect to be given the necessary instructions about what to do with these medications in the days before your flexible sigmoidoscopy. If you are not given this information, then please ask.
It will be helpful to the endoscopy team if you bring all your medications (or at least a list of these indicating the dose and how frequently they are taken) with you when you attend for your flexible sigmoidoscopy.
Prior to admission
In order to have a good clear view of the bowel it is essential that the left side of your large bowel is completely empty.
You will receive an enema. A small tube is placed into the rectum and a small amount of fluid introduced. You are asked to hold onto this for a few minutes so that it stimulates the need to pass a bowel motion and clear the bowel.
Before attending you will be informed whether the enema should be given at home before leaving for the endoscopy unit or whether it will be given in the endoscopy unit after you have arrived. If you are expected have the enema at home this will be organised and supplied in advance.
Important
It is extremely important that you follow the instructions exactly. If these instructions are not followed your flexible sigmoidoscopy may fail and be a waste of time or even be cancelled.
The effect of the enema means that you will need quick access to a toilet for up to an hour. If you get any severe abdominal pain, contact the endoscopy unit or your doctor.
Occasionally an additional enema may be required to ensure a clear left side of the bowel. You must keep taking any essential prescribed tablets.
What happens on the day of the procedure?
Your appointment letter gives a time for you to arrive at the Endoscopy unit so that all the administrative and clinical checks can be performed before your procedure takes place.
Please note that although we do our best to work to appointment times the variable nature of the procedures undertaken in the endoscopy unit mean that you may experience a delay. Please be patient and bring something to occupy yourself during this time.
When you arrive at the endoscopy unit you will be shown to your admission area and asked to change into a gown. Please feel free to also bring a dressing gown and slippers with you.
If you have not already done so, you will be asked to sign your consent form, giving the endoscopist permission to perform the procedure. This is done after you have had a final chance to ask questions and the clinician performing the test has ensured that the procedure remains appropriate for you.
If we expect you to self-administer the enema preparation (liquid inserted into the lower bowel through the anus to clear out the lower portion of the bowel) before setting off from home, then this will have been given to you (along with the necessary instructions) in advance of the procedure. Most patients are given an arrival time in advance of their procedure appointment so that endoscopy nursing staff can give the enema in a private room about 30 minutes before the procedure.
You will be asked to decide whether you wish your flexible sigmoidoscopy to be undertaken with Entonox (“gas & air”), conscious sedation or both of these.
Entonox or conscious sedation?
A flexible sigmoidoscopy is not a pleasant experience but usually only lasts approximately 15 minutes. You may go home yourself, return to work and drive if you do not have sedation.
You may wish to leave the final decision about sedation until after further discussion when you arrive in the endoscopy unit. However, if you choose sedation, you will need to be able to make the required arrangements before the procedure can go ahead.
These requirements are outlined later in this document (Discharge section), but the most important stipulation is that if you have sedation a responsible, supervising adult must take you home by car or accompany you in a taxi and stay with you for at least 12 hours.
Conscious sedation
If you choose to have sedation you will have a small plastic cannula inserted into a vein on your hand or arm. Medication can be given through this to make you relaxed for the procedure.
You will be conscious and awake throughout the test and may well have some awareness and memory of the test. Giving you sedation (often with the addition of analgesic, or pain relief medication) helps to ensure that this is not a distressing experience.
Entonox (“gas & air”)
Some patients choose to have a flexible sigmoidoscopy without sedation. You can receive Entonox (a nitrous oxide containing gas) to breathe in through a mouthpiece during the procedure to reduce the amount of discomfort.
Entonox leaves your body within a few minutes with no lasting effect. It is usually possible for you to drive yourself home after the procedure (after a 30 minute wait) if you wish to do so.
Entonox can also be used in combination with intravenous pain relief and sedation medication.
What happens in the endoscopy procedure room?
- You will be asked to confirm your name and other details and the endoscopy team will make sure you and they agree that you have attended for the correct procedure.
- You may be asked to remove any false teeth, plates, or dentures. This is particularly the case if you do not sleep with these in place.
- You will then be asked to lie on your left-hand side on a couch.
- A nurse will make sure of your comfort and dignity at all times.
- If conscious sedation has been chosen, you will be given the intravenous sedative and / or pain relief injection through the cannula in your arm.
- A small tube will be placed in your nose to provide oxygen and a clip put on your finger to continuously check the oxygen level in your blood.
- The procedure will then be performed and you might be given more sedation, if required.
- Your blood pressure will be recorded intermittently during the procedure.
- If you want the procedure to be stopped at any time, then please discuss this with the endoscopy team. The endoscopist will stop the procedure and if you are still unable to continue, they will end the procedure as soon as it is safe to do so.
- During the examination your tummy may feel bloated and slightly uncomfortable as a small amount of gas is pumped into the bowel to allow all the folds to be fully examined. This gas quickly disperses within a few hours.
- A number of photographs are standardly taken during an examination and taking these does not mean that anything is wrong. Abnormalities are often also photographed to inform the doctors responsible for your care. These photographs are often added to the endoscopy report. In almost all cases you will be offered a copy of your report to take home. Separate copies will be sent to your General Practitioner and any other doctors involved in your care.
What risks are associated with flexible sigmoidoscopy?
The endoscopy team always try to ensure that the procedure is as safe as possible. Unfortunately, even when all precautions are taken and everything is done properly complications can still happen. The quoted risks of complications may vary according to your particular circumstances. Your doctor will be able to indicate if your risk is higher or lower than the quoted rate.
Serious complications occur extremely infrequently but flexible sigmoidoscopy can result in the development of heart problems (a heart attack where a portion of heart muscle may die), a stroke (an interruption in the blood supply to the brain causing a loss of function) or exceptionally even death with a risk of approximately 1 in 25,000.
Missed lesion
Very occasionally lesions (abnormal areas) in the bowel may be missed. This is particularly so if the bowel preparation is poor. The endoscopist may occasionally have to organise a repeat procedure or alternative investigation if the bowel preparation is not adequate.
Sedation
Sedation can occasionally cause problems with breathing, heart rate and blood pressure. If any of these problems do occur, they are normally short lived but may require corrective treatment by the endoscopy team.
Exceptionally, reversal of the pain relief medicine or sedation may be required.
The procedure
Perforation (or tear of the lining) of the bowel has a risk of approximately 1 in every 15,000 examinations. An operation is often required to repair the hole. The risk of perforation is higher with polyp removal but still much less than 1 in 100.
Bleeding may occur at the site of biopsy in less than 1 in 1000 cases or polyp removal with a risk of approximately 1 for every 50 procedures where this is performed. Such bleeding is usually minor and will either simply stop on its own or if it does not, be controlled by cauterisation, injection treatment or the use of clips. Sometimes bleeding can happen up to two weeks after polyp removal.
If you take blood thinning medication, then a significant sized polyp would not normally be removed at your flexible sigmoidoscopy and you may need to return at a later date for a further flexible sigmoidoscopy or full colonoscopy (camera test to look at the whole of the large bowel) after stopping such medication for a few days.
What happens after the procedure?
When the flexible sigmoidoscopy is completed you will be transferred to the recovery area and monitored by the healthcare team until you are ready for discharge home.
After the procedures you may have some discomfort due to gas put into the upper gut and bowel during the test. You will be encouraged to pass wind and any discomfort should disappear within a few hours.
It would be unusual to have any significant pain the day after any endoscopic procedure. If you have increasing amounts of pain, or this is severe, you should contact the endoscopy unit where your procedure was performed within opening hours – details at end of leaflet.
Outside of these times you should make contact for urgent medical advice from your GP practice, local walk-in centre or, in severe cases, by attending the Accident & Emergency department at your local hospital.
You should receive a copy of your report and a discharge instruction sheet. You should be informed about the next step in your care and how you will be informed of the result of any biopsies that have been taken. Usually this will either be by letter or at a forthcoming out-patient appointment.
Discharge advice
If you have had sedation a responsible supervising adult should take you home by car or accompany you in a taxi and stay with you for at least 12 hours.
For at least 24 hours following a colonoscopy under sedation (and until you have returned to your previous state of full function and co-ordination) we must insist that you do not:
You must not go home alone, even by taxi. You must arrange an escort.
You must be able to arrange for someone to be with you at home to supervise you until next morning.
You must not drive any vehicle for 24 hours.
It is also unsafe to operate any potentially harmful equipment or machinery and you should not sign any legal documents for the same period.
If you were to take alcohol within the same period, it would have a more pronounced and unpredictable effect. You should avoid this.
Contact information:
- James Cook University Hospital (JCUH) appointments:
Telephone 01642 282576 (Monday to Friday, 8am to 6pm) - Friarage Hospital Northallerton (FHN) appointments:
Telephone 01609 763276 (Monday to Friday, 8.30am to 5.30pm) - Email: [email protected]
Patient experience
South Tees Hospitals NHS Foundation Trust would like your feedback. If you wish to share your experience about your care and treatment or on behalf of a patient, please contact The Patient Experience Department who will advise you on how best to do this.
This service is based at The James Cook University Hospital but also covers the Friarage Hospital in Northallerton, our community hospitals and community health services.
To ensure we meet your communication needs please inform the Patient Experience Department of any special requirements, for example; braille or large print.
T: 01642 835964
E: [email protected]