
Bariatric Surgery
Laparoscopic gastric bypass
A gastric bypass is a life changing operation. It is used to help people to lose weight and improve their health. Losing weight lowers the risk of developing medical problems associated with obesity, for example, high blood pressure, diabetes, arthritis, breathing problems and asthma.
The gastric bypass makes your stomach smaller and allows food to bypass part of the small intestine. The operation will change the amount that you can eat on a permanent basis. You will also need to take daily calcium plus daily vitamin and mineral supplements for the rest of your life – and have a vitamin B12 injection on a three-monthly basis for life.
The surgery makes it easier for you to lose weight as your appetite is reduced.
The surgery is done laparoscopically, commonly known as “keyhole” surgery. This means that you will be up and about soon after surgery and should make a speedy recovery.
How does it work
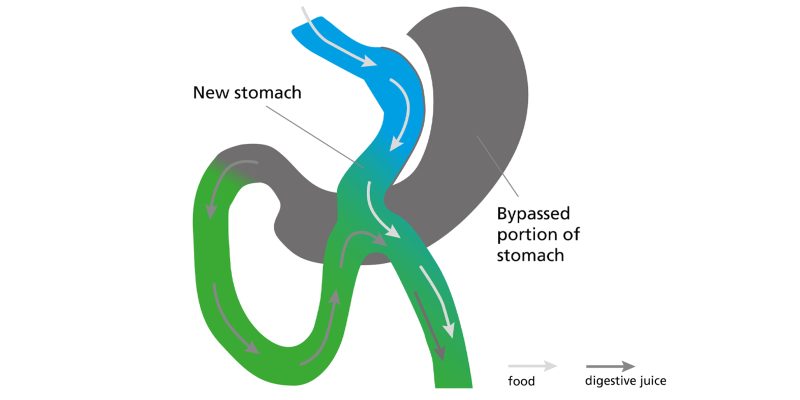
The operation involves making a new smaller stomach and bypassing the first part of your small intestine. After the surgery, the food will go into the new stomach and will then pass into the new route bypassing the rest of the stomach.
The operation also alters some of the hormone signals from the stomach and intestine to parts of the brain that control appetite, the feeling of fullness and body weight: many patients report that following this operation they feel less like eating and feel fuller.
As the size of your stomach has been reduced, the size of your meals will need to be reduced to be appropriate for your new small stomach. Your reduced portion size combined with low fat, low sugar choices and exercise will help you to lose weight and maintain the weight lost.
One anastamosis loop gastric bypass procedure
There is one potential problem with a one anastomosis loop gastric bypass surgery.
Because the pouch is small and is joined close to the flow of digestive juices, it is possible for these juices to “reflux” up into the stomach pouch causing erosion, inflammation and painful ulceration.
Patients are carefully selected for this procedure if they are not already known to suffer with acid reflux issues. If patients go on to develop reflux post operatively, this procedure can be converted with further surgery to divert the bile to resolve this issue
How much weight can you expect to lose?
You can expect to lose between 55% and 85% of your excess weight in the first 12 to 18 months following surgery. However an excess weight loss of 100% or more is not uncommon in patients who do intensive exercising.
The amount of weight you could lose and keep off after surgery will depend also on the lifestyle changes that you make, such as increasing the amount of exercise you take and eating a healthy diet. It is important to remember that the operation will not stop from you from craving certain foods or eating what you fancy.
Women of childbearing age must not become pregnant for at least two years following gastric band surgery. After two years: if you are planning a pregnancy, please contact your specialist bariatric nurse and dieticians for nutritional advice.
What are the risks of a gastric bypass?
As with all major surgery, gastric bypass has some risks. These risks vary according to your age and other illnesses you may have.
The risk of death within the first 30 days after surgery is estimated to occur in less than 0.5% (or one in every 200 patients) having this operation. This number does not reflect the experience of our surgeons, but it is calculated on national and international averages on the base of large multicentre databases.
Other complications, listed below, happen in less than 5% of patients (or one of every 20 patients).
Complications that can occur soon after surgery
- Wound infection
This can usually be treated with a course of antibiotics and does not require hospital admission - Bleeding
You will be monitored carefully for signs of bleeding. If occurs, it can be often managed and occasionally it may require transfusions. Exceptionally, the surgeon will need to perform surgery to stop the bleeding. - Blood clots in the legs or the lungs (DVT or PE)
To prevent blood clots from forming you will be given special stockings, and an injection to thin the blood. During and immediately after your operation you will also wear special boots to prevent clots from occurring. You need to continue to wear the stockings for six weeks after your operation. Smoking significantly increases the risk of clotting. If you are a smoker, you will be advised to stop smoking before surgery. - Leaks from staple lines
This after-surgery problem is rare but serious and may require emergency surgery. A leak is usually caused by a failure of the natural healing process as all staple lines are checked at the end of the operation. If this happens, your hospital stay will be longer. Sometimes this will heal without further surgery. In the worst-case scenario, your surgeon may decide to take you back to theatre to control the leaking.
Staple lines are checked during surgery using blue dye, for this reason you may have some blue coloured staining to your mouth after your operation which is easily washed off with normal soap and water, and the first time you pass urine it may be a blue/green colour. - Abnormal contractions of the digestive system (dysmotility)
Very occasionally the new stomach may respond to surgery with frequent spasms and a temporary intolerance to food and even liquids. This is a rare and unpredictable event which may require temporary tube feeding.
Long term complications after gastric bypass surgery
Long term problems are uncommon but can include:
- Port-site hernias of the abdominal wall
- Narrowing (stricture) of the joining between the new stomach and the bowel which can make eating and drinking more difficult. This will usually settle on its own although sometimes it will need to be stretched with an endoscopy
- Hair loss or thinning in the first six months. This is a temporary side effect of the rapid weight loss and it will re-grow
- Gallstones
- Worsening of symptoms of irritable bowel disease (IBS)
- Dumping syndrome – which is caused when particularly sugary or starchy food moves suddenly into your small intestine.
How should you prepare for the procedure?
Prepare a list of written questions for your surgeon
Read information on UK patients’ group websites such as Weight Loss info
Discuss the operation with your close friends and family
Meet other patients if possible
Make healthier changes to your lifestyle
One week before the operation you will be required to follow a liver shrinkage diet
The day of the operation
You will usually be admitted to the hospital on the day of your operation. If you are diabetic, you may be admitted the day before surgery.
Once your admission is complete you will see your surgeon and the anaesthetist, and a written informed consent will be signed. You will then walk to theatres where the anaesthetist put you to sleep. You will also be given an intravenous drip so you can have fluids during the operation.
What should you expect after the procedure?
The first few hours after the operation
You will wake up in a recovery room where nursing staff will monitor you for any complications. You will have a drip in your arm. You will also be wearing stockings and have a pumping device on your legs to prevent blood clots.
As soon as you are fully awake and comfortable, you will be transferred to either the surgical ward or a higher care area if necessary, where your relatives can visit you.
You will receive painkillers to control any pain. Your surgeon will instruct you when you may start to drink water, it is important you do not have anything to drink until your surgeon feels it is appropriate for you to do so.
You will be encouraged to get out of bed as soon as possible on the day of surgery. This helps to reduce the chance of post operative complications such as blood clots in the legs or chest infections.
The day after the operation
If you have been looked after in high dependency, you will be transferred to the ward.
The amount you may drink will be increased every couple of hours until you are able to take at least one glass of water every hour. Your drip will be removed when you are drinking enough to keep you hydrated.
The following one to two days after the operation
You need to drink one 125ml glass of smooth fluid every hour when you are awake.
Day one: you will be encouraged to drink clear fluids including black tea.
Day two: tea or coffee with milk, clear soup and clear jelly.
At discharge
Pain and medication
You will be given a supply of soluble or liquid painkillers to take home with you; these should be taken regularly for the first few days. If you have no pain gradually reduce the number of painkillers you are taking. Allow soluble tablets to stop fizzing before you drink them.
You will also go home with a blood thinning injection daily for ten days to help reduce the risk of you developing blood clots. It is essential that you increase your activity as your specialist nurse and consultant have advised.
If you have been taking medication to control your blood pressure or diabetes, these will be reviewed before your discharge. Please make sure you are clear about this before you leave the hospital.
Important
Do not take any large tablets for first four weeks as they may get stuck and damage the staple line. Some tablets may need to be crushed or taken in soluble form. If in doubt, please ask your specialist.
Medication and appointment following the operation
You will need a three-monthly vitamin B injection for life (arranged via GP), you will take Lansoprazole, multi-vitamins and Adcal D3 daily for life following the operation.
You will receive a follow up out-patient appointment for six weeks following your operation. Then be reviewed again at 6 months,12 months and 2 years post operatively.
At 2 years post operatively, you are discharged back to your GP for yearly monitoring of your weight, BMI, Micronutrient blood screening and wellness review.
Wounds
Abdominal sutures will need removing by your practice nurse at 14 days after your operation.
Anti-emboli stockings
You should take them home with you and continue to wear them for six weeks, day and night, following your operation. We advise you not to fly within six weeks of your operation. If you fly soon after this, we advise you to wear stockings during the flight.
Eating and drinking
You will be given a diet information sheet. You should have this with you at all times so you know what to drink and eat and are familiar with the stages of food introduction in the next few weeks. In case of doubt you are advised to contact your dietician.
You are advised to drink at least two litres of fluid per day to help avoid dehydration and constipation, it is a good idea to obtain a water bottle so you can maintain this fluid intake whilst out of the house and overnight whilst in bed.
Washing
You can have a shower but, for at least a week after surgery, do not soak in the bath.
Driving
You may drive as soon as you can comfortably wear a seat belt and are able to perform an emergency stop (independently assessed by a close relative or a friend). You should check with your insurance company for their specific advice about driving after keyhole (laparoscopic) surgery.
Other activities
You will be able to walk straight after surgery. Try to go for a walk every day, gradually increasing the distance as you feel able. You will need approximately six weeks off work but please check with your specialist nurse.
It is advisable to avoid heavy lifting for at least two months after abdominal surgery, if you are unsure discuss with your surgeon.
You may resume sexual activity as soon as you feel comfortable.
Physiotherapy following your surgery
Breathing exercises
It is important to start doing deep breathing exercises as soon as possible after your operation. These will help to keep your lungs open and prevent infection.
Take a slow deep breath in, hold for one to two seconds, and then gently sigh out.

Coughing
It is very important to get rid of any phlegm you may have in your lungs to help prevent infection. Try a cough at least every hour after a set of deep breaths.
If you have a wound on your stomach, it would be helpful to make a cough pad to use in the first few days following surgery. You can make this by rolling up a small towel or pillow.
Place the cough pad over your stomach, support with your hands and try a good cough. It is easier to cough in an upright position. If laid in bed, try to bend your knees up to help ease the strain
Huffing
Sometimes when phlegm collects lower down in your lungs you may need to try huffing. Take a medium sized breath in and then quickly ‘huff’ the air out as if steaming up a mirror.
Practise this exercise after your deep breaths and follow with a cough.
Leg exercises
Regular leg exercises will help encourage blood flow and keep your muscles strong and supple. Try the following exercises every hour until you are walking normally again.
- Wiggle your toes
- Circle your feet briskly in both directions
- Bend each knee in turn up to your chest and then lower slowly
- Straighten your knee to tighten the muscle on the front of your thigh. Hold for the count of three
For those patients following bypass surgery
On the same day as your operation, or if not the following day, you will be helped to get out of bed and sit in the chair.
To help reduce the strain on your wounds, roll onto your side and then push your upper body up off the bed with your arms. By lowering your legs over the side of the bed at the same time you will easily move into a sitting position. After a few minutes rest you will be helped to move into a chair.
You will be encouraged to start walking as soon as possible, slowly increasing the distances.
Ideally you should aim to get up into your chair for most of the day. The more you can sit out of bed the better it will be for your breathing and keeping your chest clear.
Remember
Stop if you feel short of breath or experience pain and talk to your physiotherapist or nursing staff. Each person is an individual and the distances you can walk will vary. The staff will give you specific advice on how you are recovering.
Posture
Check your posture by standing in front of a mirror. Try to stand up straight with your shoulders back. It is common to lean forwards as this helps reduce the tension on your wound. Although this is often more comfortable, your body may become stiff in this position.
Discharge from hospital
When you go home it is important to continue with the exercises and slowly increase the distances walked. Within one or two days of returning home start to venture outside, slowly increasing the distances you can walk.
Post operative activity schedule
The walking schedule below is merely a guide to help you get back to exercise. It is a guide as everyone will differ, however your physiotherapist will discuss this with you prior to your discharge.
| Date | Week | Walking time | Walks per day | Other exercise |
|---|---|---|---|---|
| 1 | 5 to 10 mins | 2 | ||
| 2 | 10 to 15 mins | 2 | ||
| 3 | 20 mins | 2 | ||
| 4 | 25 to 30 mins | 1 |
Contact details
- The James Cook University Hospital
Tel: 01642 854505 (available 24 hours) - The Bariatric Team
Tel: 01642 835724
Email: [email protected]
Further help and information
- Weight Concern
1-19 Torrington Place, London WC1E 6BT
Tel: 020 7679 1853 (not a helpline)
www.weightconcern.org.uk
Weight Concern is a registered charity, set up to tackle the rising problem of obesity. Weight Concern has shown how psychologists, dieticians and exercise specialists working together can help people make the lifestyle changes they want, to control their weight.
- WLS info (Weight Loss Surgery Information and Support)
Wessex House, Upper Market Street, Eastleigh, Hampshire SO50 9FD
Tel: 0151 222 4737
www.wlsinfo.org.uk - British heart foundation
www.bhf.org.uk - Diabetes UK
www.diabetes.org.uk
Patient experience
South Tees Hospitals NHS Foundation Trust would like your feedback. If you wish to share your experience about your care and treatment or on behalf of a patient, please contact The Patient Experience Department who will advise you on how best to do this.
This service is based at The James Cook University Hospital but also covers the Friarage Hospital in Northallerton, our community hospitals and community health services.
To ensure we meet your communication needs please inform the Patient Experience Department of any special requirements, for example; braille or large print.
T: 01642 835964
E: [email protected]